Abstract
Background: The International Prognostic Index (IPI) was first described in 1993 and is the most widely used prognostication tool in diffuse large B-cell lymphoma (DLBCL). Five independent risk factors for OS: age (≤60 yrs versus >60 yrs), stage (I/II versus III/IV), number of extranodal (EN) sites (≤1 versus >1), performance status (PS) (0-1 versus ≥2) and serum lactate dehydrogenase (LDH) (normal versus elevated) were used to design a prognostic model which stratified patients into 4 prognostic groups according to the number of risk factors present: low (0-1), low-intermediate (2), high-intermediate (3), and high-risk (4-5); predicting 5-yr OS rates of 73%, 51%, 43% and 26% and 5-yr relapse-free survival (RFS) rates of 70%, 50%, 49%, 40% respectively. For patients aged ≤60 yrs 3 risk factors (stage, PS and LDH level) remained independently significant for OS, and an age-adjusted (aa) model (the aa-IPI) was proposed which predicted 5-yr OS for the low (0), low-intermediate (1), high-intermediate (2) or high-risk (3) groups of 83%, 69%, 46% and 32% respectively (Shipp et al, 1993). The British Columbia Cancer Agency re-evaluated the role of IPI in the rituximab era in their registry-based cohort of 365 patients in 2007. Although the IPI remained predictive, only 2 (rather than 4) prognostic groups were identified and the authors recommended use of the Revised-IPI (R-IPI) where redistribution of the absolute number of IPI risk factors better stratified patients into 3 prognostic groups: very good (0) good (1,2) and poor (3-5) (Savage et al, 2007). However, a subsequent analysis of pooled data from 3 prospective trials (Ziepert et al, 2010) confirmed that the IPI remained highly predictive of outcomes in the rituximab era. Here we report an evaluation of prognostic indices within the UK NCRI R-CHOP 14 vs 21 prospective trial cohort (Cunningham et al, 2013).
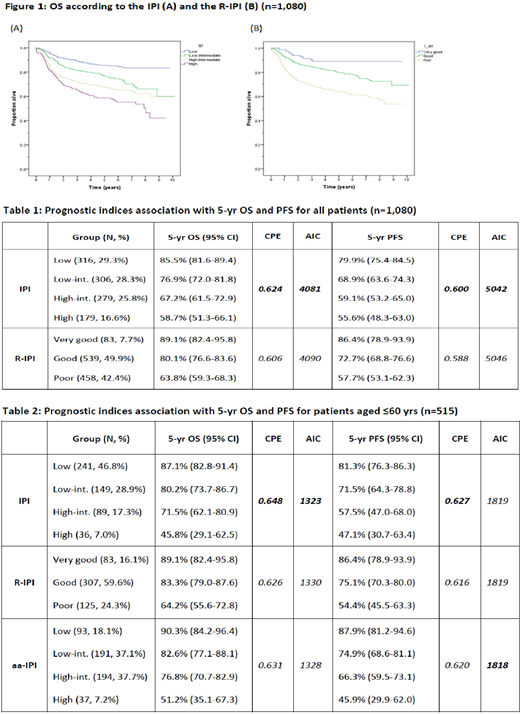
Methods: The IPI and R-IPI were applied to the R-CHOP 14 versus 21 trial cohort (n=1,080) and for the subgroup of patients aged ≤60 yrs (n=515) and correlated with OS and progression-free survival (PFS). For patients aged ≤60 yrs the aa-IPI was applied in addition. It was not possible to evaluate the NCCN-IPI in our cohort as absolute LDH values were not collected at enrolment. The association between baseline clinical factors (age, gender, PS, stage, presence of >1 EN site of disease, presence of an elevated LDH, disease bulk and B symptoms) and patient outcomes were investigated in univariable and multivariable analysis (MVA). Performance of the prognostic indices was compared using the Concordance Probability Estimate (CPE) and Akaike's Information Criterion (AIC): CPE evaluates discriminatory power to assess the strength of statistical models (higher values indicate better discrimination); AIC estimates the quality of statistical models relative to each other in terms of fitting the data (lower values indicate a better model fit).
Results: After a median follow-up of 6.5 years, both the IPI and R-IPI were significantly associated with OS (Figure 1) and PFS; the IPI performed better than the R-IPI for OS and PFS in terms of discrimination and model fit (Table 1). All IPI factors were significantly associated with OS, and remained in MVA with the exception of disease stage. For patients aged ≤60 yrs, the IPI, R-IPI and aa-IPI were all strongly associated with OS and PFS; the IPI performed best overall of the 3 prognostic indices in terms of discrimination and model fit (Table 2). All individual IPI risk factors, excepting stage, were again found to be significantly associated with OS in MVA for patients aged ≤60 yrs.
Conclusion: For the entire DLBCL cohort both the IPI and R-IPI identified meaningful prognostic groups for OS and PFS. Although the IPI outperformed the R-IPI, neither index identified a patient subgroup with an OS of <50% at 5 years. When the analysis was limited to patients aged ≤60 yrs all 3 indices were prognostic, however the IPI performed best overall and was the only risk model to detect a patient subgroup with a 5-yr OS of 45.8%. Our findings suggest that neither the R-IPI nor aa-IPI offer an improvement over the standard IPI in predicting outcomes in DLBCL. Furthermore, our analysis highlights the lack of precision of the traditional prognostic indices in identifying very poor risk patients treated in the rituximab era.
Cunningham:Roche pharmaceuticals: Research Funding. Hawkes:Bristol Myers Squibb: Other: Speaker fee, Research Funding; Merck KGA: Research Funding; Astra Zeneca: Research Funding; Merck Sharpe Dohme: Research Funding; Celgene: Other: Advisory board, Research Funding; Takeda: Other: Speaker fee; Merck: Other: Advisory board; Roche: Other: Speaker fee; advisory board. Pocock:Kent & Canterbury Hospital: Employment. Ardeshna:Celgene: Membership on an entity's Board of Directors or advisory committees; ADC Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Roche: Membership on an entity's Board of Directors or advisory committees, Other: Conference expenses, Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees. Radford:Celgene: Research Funding; Takeda: Consultancy, Research Funding, Speakers Bureau; ADC Therapeutics: Consultancy, Research Funding; Seattle Genetics: Consultancy, Speakers Bureau; GlaxoSmithKline: Equity Ownership; Novartis: Consultancy, Speakers Bureau; AstraZeneca: Equity Ownership; BMS: Consultancy, Speakers Bureau; Pfizer: Research Funding. McMillan:Celgene: Honoraria, Other: travel support; BMS: Honoraria; Amgen: Honoraria; Takeda: Other: travel support; Roche: Consultancy, Honoraria, Other: travel support; Pfizer: Research Funding; MSD: Honoraria. Johnson:Janssen: Consultancy, Research Funding; Epizyme: Consultancy, Honoraria, Research Funding; Boeringher Ingelheim: Consultancy; Kite: Consultancy; Incyte: Consultancy; Bristol-Myers Squibb: Honoraria; Takeda: Honoraria, Travel, accommodations, expenses; Novartis: Honoraria; Celgene: Honoraria; Eisai: Research Funding; Zenyaku Kogyo: Other: Travel, accommodations, expenses; Genmab: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal